From asthma research to better treatment for cystic fibrosis complications?
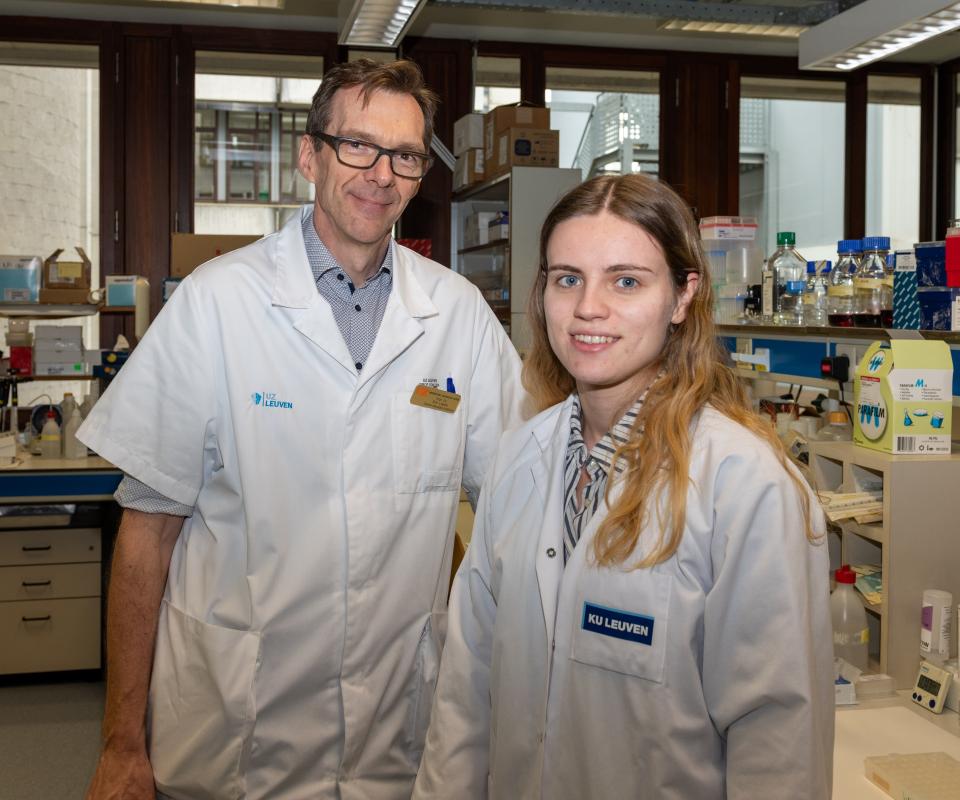
A significant number of cystic fibrosis (CF) patients experience a dreaded complication caused by an overreaction to fungal spores in their airways. Could a recent breakthrough in asthma research improve understanding of this CF complication and lead to a better quality of life for patients? Pulmonologist Eva Van Braeckel, a professor at Ghent University (UGent) and doctor at Ghent University Hospital (UZ Gent), tells us about her research collaboration with colleague Bart Lambrecht, a professor at Ghent University's Flemish Institute for Biotechnology (VIB-UGent) and doctor at UZ Gent, for which the team is benefiting from financial support provided by the Alphonse and Jean Forton Fund, managed by the King Baudouin Foundation, and the Belgian Cystic Fibrosis Association.
Breathe in. Breathe out. We do it millions of times, rarely pausing to consider how many microorganisms we breathe in and – as long as we have healthy lungs – mostly breathe out again. For people with CF, breathing in and out is not so carefree because the layer of thick mucus in their lungs is an ideal biotope for such microorganisms, including bacteria and fungi. To use the medical jargon, their airways – which gradually become more and more damaged by the thick mucus and frequent infections – are colonised by microorganisms.
"In some cases those microorganisms remain inactive, in others they cause infections to flare up. In an estimated 10 to 20% of CF patients, the damaged airways overreact to inhaled fungal spores, in a kind of allergic reaction," Dr Van Braeckel explains. "When these patients are exposed to fungi, which can be found all around, it triggers an inadequate inflammatory response, with the defensive reaction itself causing damage."
Arduous treatment
This is the dreaded ABPA, or allergic bronchopulmonary aspergillosis – 'dreaded' because diagnosis is very difficult and also because it is a condition requiring very arduous treatment. "There is no unambiguous 'marker' for ABPA, no single substance that proves that it's present," Dr Van Braeckel explains. "The presence of the fungus itself is inconclusive because many patients have it in their airways without developing ABPA. So when we see a patient whose lung function is deteriorating and who has various medical problems, it is hard to identify the cause. Only after other explanations have been ruled out do we settle on ABPA."
Once the diagnosis has been made, the treatment is almost as gruelling as the disease itself. "Generally we have to treat the symptoms with cortisone because of very hard 'plugs' of mucus clogging the airways. This has significant side effects, such as accelerated development of diabetes and osteoporosis, not to mention psychological effects."
Two things are therefore needed: a quicker and easier way of making the diagnosis and a treatment with fewer side effects.
Crystals melting like snow
Dr Van Braeckel hopes that she and those working with her on this research are on the right path. She stresses the importance of multidisciplinary collaboration with the team of Prof. Dr Bart Lambrecht (VIB-UGent and UZ Gent), which specialises in asthma and inflammation research. "They recently made a major breakthrough, working out the structure of crystals that play a key role in asthma and developing antibodies to dissolve these crystals. Seeing crystals melting like snow in the sun is truly spectacular."
The link between asthma and cystic fibrosis? These same 'Charcot-Leyden crystals' are found in large numbers in the mucus plugs of patients with ABPA. "The first research question is: Could the presence of the crystals be a sign that the patient has ABPA? That would make diagnosis much easier, because we already have a reliable technique for detecting the crystals. The second question is: Does this provide a pathway to a treatment with the same antibodies?"
Ex-vivo research
Dr Van Braeckel and her fellow researchers are using the research budget provided by the Alphonse and Jean Forton Fund and the Belgian Cystic Fibrosis Association to finance an ex-vivo study using real patient material, i.e. sputum or mucus from deep down in the airways, which is then examined outside the body, in the laboratory, to determine both the exact composition of the plugs that block the airways and the effects of the antibodies. If the results are encouraging, this will be followed by clinical research into the effects of the substance when administered to a patient, for example by being sprayed as an aerosol into the airways.
The ex-vivo study sounds simpler than it actually is. "The techniques to fully understand the composition of the plugs and the development of the antibodies require substantial efforts and resources. Ideally, to demonstrate the link between the crystals and ABPA, we have to be able to get the material from deep inside the airways, which often means using a scan and a special ultra-fine bronchoscope to look for existing plugs. That's because we have to be sure which type of mucus is typical for ABPA. In addition, research needs to be carried out on a control group of individuals who have a lot of fungal spores in their lungs but no ABPA."
Time frame
The time frame will depend on how many patients present with ABPA and want to participate in the study. It will probably be two to three years before there are enough participants, and collaboration with other CF centres is also being set up for this purpose. If a drug does emerge form the research, it will be at least 10 years down the line. "With a rare disease like CF, it's common for a relatively large number of patients to be invited to receive treatment already in the research phase."
"When we see a patient whose cystic fibrosis is deteriorating, it is often hard to identify the cause. There is a need for better diagnosis of allergic reactions to fungi."
The search for ways to tackle CF at source is still very much ongoing and has yielded many promising results in recent years. At the same time, researchers are continuing to look for a treatment for the complication ABPA. "Treatments called CFTR modulators are being developed which act on the protein defects that cause CF in 90% of patients. Patients who are sensitive to ABPA and who are already receiving such causal treatments – whether or not as part of a clinical trial – experience a considerable reduction in thick mucus and infections, but the ABPA remains a problem. Due to the accumulated damage, the airways continue to react hypersensitively to fungal spores. So while it may be possible, within a few years, to directly tackle the underlying cause in young children, there will still be many 'older' patients – six out of ten people with CF are adults – for whom a less arduous treatment for ABPA would be a very welcome development."
About the sponsors
This is the second time that the Forton Fund and the Belgian Cystic Fibrosis Association join forces for a joint funding of projects. Six university research groups are receiving financial support for which nearly €1.4 million was earmarked. The Alphonse and Jean Forton Fund was created more than 20 years ago to support research into cystic fibrosis and related diseases. Over the years, this philanthropic fund, managed by the King Baudouin Foundation, has provided over €9 million in funding to research projects. The Belgian Cystic Fibrosis Association is the patient organisation of and for people with cystic fibrosis and their families in Belgium. The association, founded in 1966, initiates activities aimed at empowering patients and their families or improving their quality of life and awards grants to innovative research projects.
Other stories
Inspiring engagement!

Pancreatic cancer: gradually untangling a complex knot
Health Research
“In families where there are more cases of pancreatic cancer, we are also seeing an association with colon and breast cancer.”
New perspective on DNA variations leads to explanation for rare disease
Health Research
“We have shown that it is also worthwhile to look at the variants just before and just after genes.”
Other calls

Belgian Heart Fund - Clinical research in cardiology
Support for clinical research in cardiology.
Ongoing
Belgian Heart Fund - Multicentre Randomised Clinical Trials in cardiology
Support for multicentre randomised clinical trials in cardiology.
Ongoing
Belgian Heart Fund - Basic research in cardiology
Support for basic research in cardiology.
OngoingOther publications
Other philantrophy
Other press releases